The eighth Citizens' Panel survey was carried out in November 2021. We asked questions about dentistry services, urgent care services, planned care services, and the remit of the Patient Safety Commissioner.
At the time of this survey in November 2021, there are 953 Panel members from across all 32 local authority areas.
A total of 599 responses (63% response rate) were received, either by post, email or by telephone. This level of return provides data accurate to +/-4.0% at the overall Panel level. In this report we do not report results broken down into sub-categories (for example, gender or age) as they are not statistically significant. All comparisons that are made in this report are statistically significant, unless otherwise stated.
Key findings
Dentistry services

When thinking about the health of their mouth, being pain free (74%) was most important to respondents, followed by having healthy teeth and gums (66%). In terms of visiting their dentist, being able to get access to treatment when needed (87%) was most important, followed by getting check-ups at regular intervals (79%).
The potential cost of dental treatment was most commonly noted as a barrier to visiting the dentist (44%) followed by difficulty in getting an appointment (29%) and anxiety about visiting the dentist (21%). Over one quarter of respondents, (27%) said that nothing stops them from visiting their dentist.
The majority of respondents (84%) said that yes, they do feel they will be able to access the dental services they want over the next year. However, just 18% said they felt they would be able to access dental services within the normal time frame whilst the other 66% said they believed they would only be able to access dental services in certain circumstances. For most participants, their preference for accessing dental services is by visiting their own dental surgery (94%).
An area identified for improvement is raising awareness on how to complain about dentistry services. Almost two thirds of respondents (62%) said that they would not know how to raise a complaint about a dental professional if they needed to. 21% said they might know how to raise a complaint and just 17% said they would know how to raise a complaint. Those who would or might know how to make a complaint were most likely to either use the complaints procedure within their local dental practice (84%) or raise their concern with the dental professional in question (80%) which is encouraging.
Recommendations:
As a result of these findings, we make the following recommendations to Scottish Government, General Dental Council and NHS dental services:
- That any reform of dental care by Government and the NHS continues to support people to be pain free and to have healthy teeth and gums rather than focus on, for example, cosmetic treatment.
- That access to treatment for patients, including to check-ups, is prioritised by dental teams as COVID-19 safety restrictions lift; and that NHS and Scottish Government continue to support dental teams to do this. The Scottish Government should also be mindful of the cost of dental treatment as a barrier to accessing dental services in future policy decisions.
- That NHS and Government continue to support dental teams to provide timely care as best they can within the current COVID-19 restrictions.
- That any reform of NHS dental services ensures visits to patients’ dentists remain a significant part of the service.
- That dental teams ensure all patients are aware of how to make a complaint should they need to, and that Scottish Government, NHS Scotland and the General Dental Council continue to support local resolution of complaints whenever appropriate.
Urgent care services
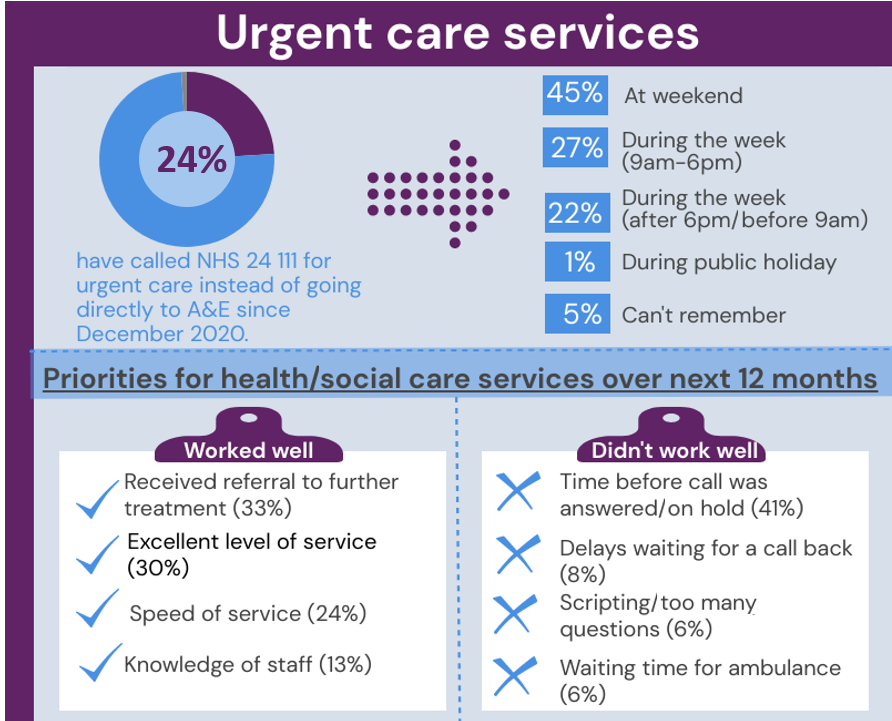
Almost one quarter of respondents (24%) have called NHS 24 111 for urgent care instead of going directly to A&E since December 2020. When thinking about what worked well in that experience, 33% said that they received onward referral for further treatment, 30% noted that the service had been excellent and 24% noted the speed of service.
Conversely, when asked what had not worked so well, the most common issue noted was the time taken for the phone to be answered (41%). Based upon their experience, the most common suggestion for improvement to this service was to have more call handlers which, it was believed, would allow a quicker response or less time on hold (41%).
When asked what is most important when needing medical help quickly but the situation is not immediately life threatening, respondents’ top priority was getting the right care and advice (74%) followed by getting care quickly and easily (67%).
NHS 24 111 was the source that the greatest proportion of respondents (56%) would turn to if they needed to get medical help for someone quickly and their situation was not immediately life threatening.
In terms of attitudes towards NHS 24 111 as a way of accessing urgent care, 56% said that they were very positive or positive about this new way of accessing urgent care compared to 16% who said they were very negative or negative. This is a positive response towards the new system with good understanding of the aims to reduce waiting times, keep A&E free for those who need it and make better use of resources.
Recommendations:
As a result of the findings on urgent care we make the following recommendations to the Scottish Government and NHS boards:
- Continue with current marketing materials to increase awareness of how to access the right care at the right time.
- Continue with current strategy to avoid unnecessary attendances to A&E by strengthening alternative pathways which will ensure people can be seen in the right place and A&E is kept free for those who need it.
- Continue to build with urgency, sufficient workforce capacity and capability, optimally aligned to meet timely and responsive urgent care demand 24/7 - across in-hours, out-of-hours, weekends and public holiday periods.
- Further consideration to the existing media campaign to ensure the public are aware that by accessing the Redesign of Urgent Care (RUC) pathway it does not preclude a face to face contact where this is deemed clinically required.
- Promote data sharing between organisations and services to ensure people receive positive and clear outcomes from accessing the RUC pathway through 111.
Planned care services
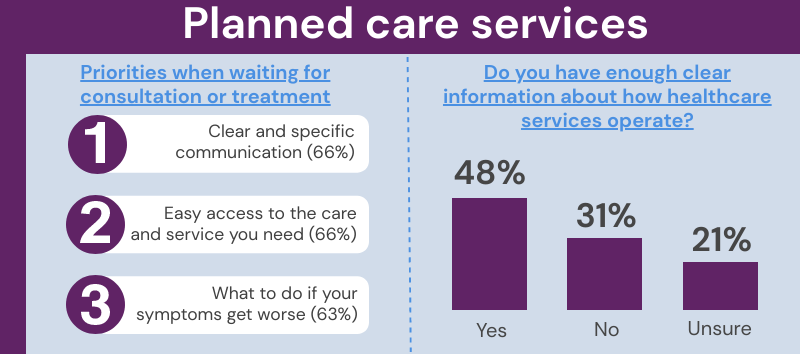
There were 3 key themes that respondents believed should be prioritised for people waiting for consultation or treatment: clear and specific communication (66%), easy access to the care and service you need (66%) and what to do if your symptoms get worse (63%).
In terms of what matters to respondents themselves when waiting for a consultation or treatment, the amount of time they have to wait, or knowing how long they will have to wait was most important to respondents (56%), followed by communication (18%), clear information on what to expect (15%) and having a contact or knowing what to do if the condition worsens when waiting (15%).
When asked if, in their experience, they have enough clear information and understanding about how the healthcare service operates between GP services, Accident and Emergency and planned care, just under half of respondents (48%) said ‘yes’ 31% said ‘no’ and 21% were unsure.
Almost two thirds of respondents (64%) agreed that ‘more could be done to improve people’s understanding of what to expect when having a planned consultation or hospital treatment’.
Recommendations:
Based on the results for planned care we make the following recommendations to the Scottish Government and NHS boards:
- Undertake a marketing campaign to raise awareness amongst the general population on how the health service operates between GP services, A&E and planned care. In addition, improve people’s understanding of what to expect when having a planned consultation.
- Develop a policy which ensures an efficient process for regular communication for those waiting for a planned consultation.
The role of the Patient Safety Commissioner
The Scottish Government is committed to establishing a Patient Safety Commissioner in Scotland. This commitment has come about as a result of First Do No Harm: The Report of the Independent Medicines and Medical Devices Safety Review (the Cumberlege Review). The review examined how the healthcare system in England responds to reports about harmful side effects from medicines and medical devices, for example pelvic mesh implants, and made recommendations on how to respond to concerns more quickly and effectively in the future across the UK. The report recommended the appointment of a Patient Safety Commissioner and the Scottish Government is committed to creating this role. We envisage that the Commissioner would be independent of Government and the NHS, and have a statutory responsibility that would:
- champion the value of listening to patients, and
- promote users’ perspectives in seeking improvements to patient safety around the use of medicines and medical devices.
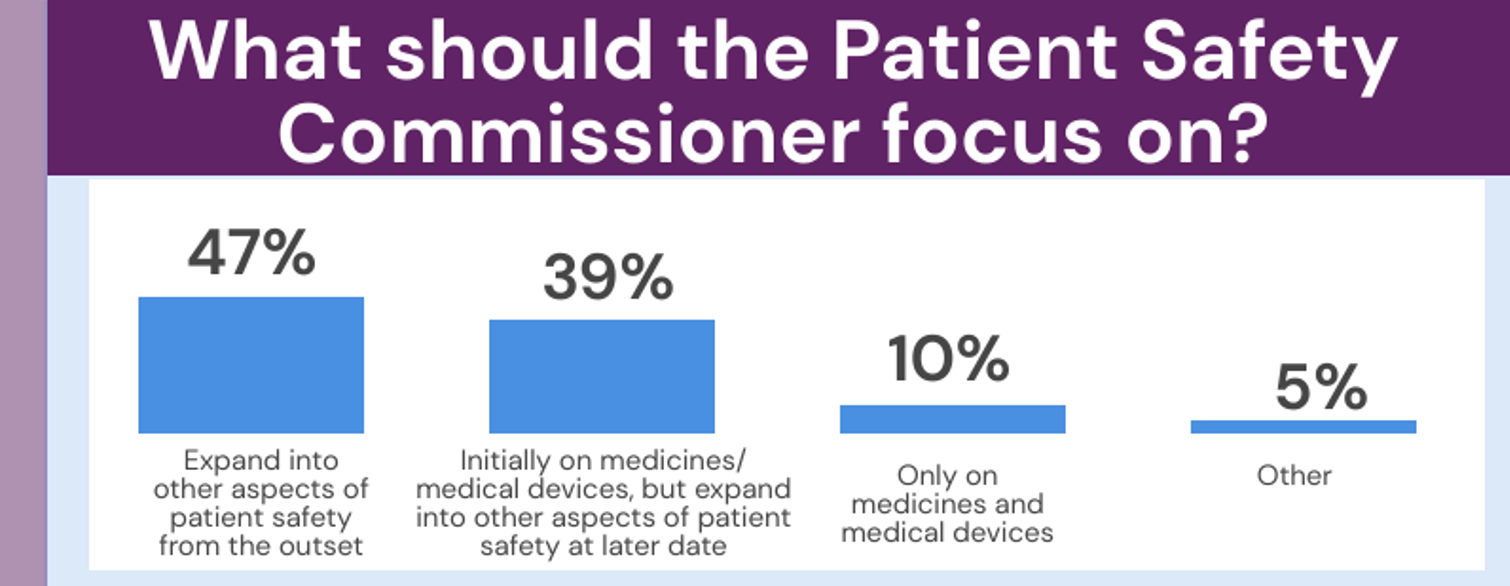
When asking the Panel what they believed the Patient Safety Commissioner should focus on, the most common option selected was that the Patient Safety Commissioner should expand into other aspects of patient safety from the outset such as surgical errors or harm coming to patients because of falls (47%). This was followed by 39% selecting that the Patient Safety Commissioner should initially focus on medicines and medical devices but expand into other aspects of patient safety at a later date, such as surgical errors or harm coming to patients because of falls.
Recommendation:
Based on the results for the Patient Safety Commissioner, we make the following recommendation to the Scottish Government:
- The Scottish Government should establish the Patient Safety Commissioner in a way that does not prevent the office from expanding to consider other areas of patient safety that are not mentioned in the Independent Medicines and Medical Devices Safety Review.
Impact
The office of the Cabinet Secretary for Health and Social Care told us:
“Mr Yousaf has noted that this is very valuable feedback and officials will want to consider the results of the Citizens' Panel in terms of further policy development.”
More specifically, in terms of the 4 topics covered by the survey, short-term impact and commitment to using the results to influence healthcare policy and services are noted below. These impacts have been fed back from topic sponsors in the Scottish Government.
Dentistry
The Citizens' Panel results have been discussed at the national Directors of Dentistry sessions, and locally with some individual NHS boards and also cited in some briefings.
The Scottish Government is in the process of designing a new model of care for Dentistry, and the results are part of this continuous loop.
The General Dental Council (GDC) has referred to our Citizens' Panel involvement in discussions with Cabinet Secretary and at presentations with various stakeholders.
In a blog post, Working with partners; listening to patients, the GDC highlights its work with the Citizens' Panel.
The GDC has also told us that the statistical rigour of the Citizens' Panel findings has helped to ensure that the recommendations have been taken seriously internally.
Planned Care
Feedback from the report was provided to progress changes in communication with patients for inpatient/day case treatments.
The results informed the summary report and highlighted key themes in Waiting Times Guidance review.
The findings were discussed with Cabinet Secretary for Health and Social Care to aid changes in patient communication and launch of online platform for patients to access information on planned care waiting times.
For the Waiting Times Guidance review, this helped to inform the patient perspective and what focal points should be of review. This will help in setting up patient and public engagement groups.
Redesign of Urgent Care
Citizens' Panel 8 results have supported the progression of the Redesign of Urgent Care programme. The findings informed our approach to marketing materials to increase awareness of how to access the right care at the right time.
This programme of work feeds into the Urgent and Unscheduled Care Collaborative that will see health boards implement a range of measures to reduce A&E waiting times and improve patient experience.
Feedback from the report will inform the Redesign of Urgent Care programme external evaluation which is in early development.
The findings were discussed with the Cabinet Secretary for Health and Social Care to showcase the impact of the Redesign of Urgent Care programme through the use of respondents using NHS 111 as a way of accessing urgent care.
Findings were shared with local RUC teams and the Strategic Advisory Group for Redesign of Urgent Care, and the importance of strong public messaging and workforce alignment was reaffirmed.
Patient Safety Commissioner
The question and subsequent responses gave good evidence to support the preparation of legislation to establish a statutory Patient Safety Commissioner, independent of the NHS and government.
The Scottish Government has used the findings to support its policy proposals and the option for legislating.
A summary of the findings was cited in the Policy Memorandum to the Patient Safety Commissioner for Scotland Bill, which was introduced to the Scottish Parliament on 6 October 2022 and passed on 27 September 2023.
Feedback from the survey influenced the scope of the Patient Safety Commissioner in the Bill.