The fourteenth Citizens' Panel survey was carried out between June and September 2024.
The survey asked questions on two topics:
- Realistic Medicine and Value Based Health and Care
- NHS Reform
A total of 545 responses (50% response rate) were received, either by post, email or by telephone. This level of return provides data accurate to +/-4.2% at the overall Panel level. In this report we do not report results broken down into sub-categories (for example, sex or age) as they are not statistically significant. All comparisons that are made in this report are statistically significant, unless otherwise stated.
Realistic Medicine and Value Based Health and Care
It was explained to Panel members that Realistic Medicine and Value Based Health and Care focus on the need to deliver better outcomes for people while making best use of healthcare resources. This could be, for example, by trying to reduce waste from medicines that are prescribed but not used. Just under half (42%) of respondents said they were aware of this need and 19% had heard about Realistic Medicine before receiving this survey.
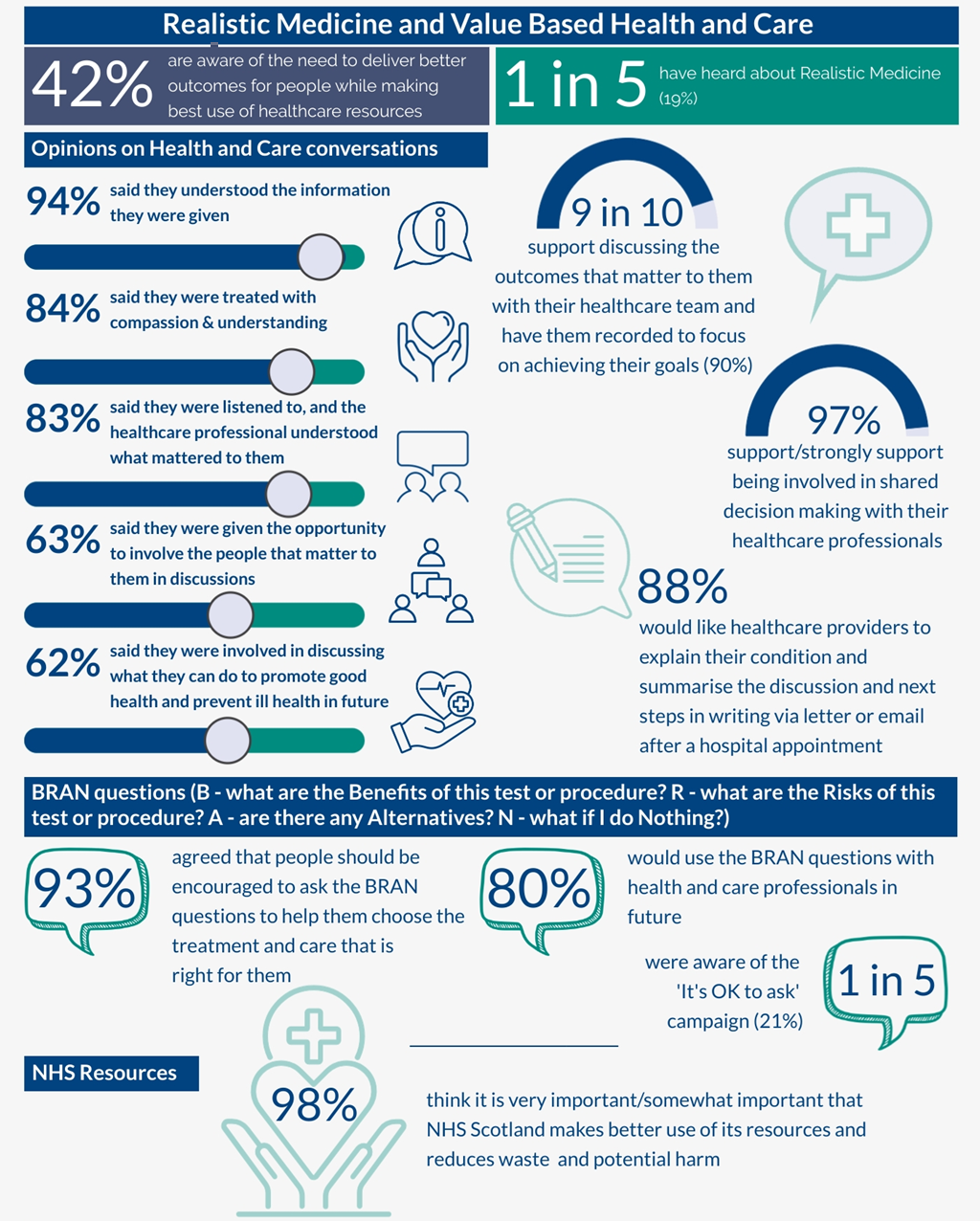
87% of respondents thought it is very important that NHS Scotland makes better use of its resources and reduces waste and potential harm, 11% said it was somewhat important and 2% had a neutral opinion on this. All respondents were asked to explain the reason for their response to this question. In response to this open question 38% of respondents who commented said that making better use of resources and reducing waste will positively impact service delivery and allow money to be spent elsewhere. A further 31% commented more generally on saving through waste reduction and 28% spoke about reducing costs and saving money. This demonstrates the public’s understanding around the impact of poor use of resources in the NHS.
Just over 4 in 10 people said that the last time they used NHS Scotland services, they received most of their treatment or advice from a GP (44%), 23% said it was from a hospital doctor and 17% said it was from a nurse. Respondents were most likely to say that they most recently saw their health professional at a GP surgery (48%), 24% said it was in a hospital and 11% said they had contact with the health professional at home by telephone.
88% of respondents agreed that following a hospital appointment with a healthcare professional they would like them to write to them to explain their condition, summarise what they discussed and agreed, and potential next steps. They would like this to be done by letter and/or email.
Respondents were asked to think about the last healthcare professional they saw within NHS Scotland and how much they agreed or disagreed with various statements. Respondents were highly likely to agree that: they understood the information they received (94%), they were treated with compassion and understanding (84%), they were listened to, and the healthcare professional understood what mattered to them (83%). However, they were less likely to agree that: they were given the opportunity to involve the people that matter to them in their discussions about their care (62%), and they were involved in discussing what they can do to promote good health and prevent ill health in the future (63%).
Panel members were asked for their opinions on the BRAN questions. These are questions which can help people to make an informed decision about the treatment and care that is right for them. The BRAN questions are:
B – What are the Benefits of this test or procedure?
R – What are the Risks of this test or procedure?
A – Are there any Alternatives?
N – What if I do Nothing?
Only 12% of respondents said that before answering the survey they had heard of the BRAN questions (86% had not heard of these questions and 2% were unsure). Despite low levels of awareness, 80% of respondents said they would use the BRAN questions with health and care professionals in future. Of those who said they would use the BRAN questions just under 4 in 10 said the questions would make them feel better informed (37%) and a further 22% said the BRAN questions were straightforward and in a simple format. Where respondents said they would not use the question set, this tended to be where they felt it would depend on circumstances (38%) or where they felt they would forget them (20%). Just over 1 in 5 respondents (21%) were aware of the NHS campaign “It’s OK to ask”. 84% said including a reminder of the BRAN questions on appointment letters and in waiting rooms would encourage them to ask them during their appointment.
Respondents said the best ways of promoting the need to focus on delivering the care that matters to people and make best use of healthcare resources was via a social media campaign (51%). This was followed by a TV campaign (48%) and adverts in NHS premises (33%). Following on from this, respondents were asked how strongly they support or oppose doing each of a variety of things to help NHS Scotland make best use of its resources, reduce waste and deliver better value care. Almost all respondents (97%) supported or strongly supported getting involved in shared decision-making with their healthcare professionals. 9 in 10 respondents supported or strongly supported discussing the outcomes that matter to them with their healthcare team and have them written down or recorded, so they can focus on achieving their goals (90%).
When asked about what matters most to them about what NHS Scotland could do to reduce waste, 23% spoke about making best use of resources to ensure effective care and minimise waste, 20% mentioned the need to reduce waste and costs and 18% mentioned the need to tackle unnecessary prescriptions and overprescribing.
Recommendations
Based on these findings, we make the following recommendations to the Scottish Government and NHS Scotland:
- Increase awareness: The public supports involving people in decisions about care and making best use of NHS resources, but awareness of NHS Scotland’s commitment to this approach is limited. Much more needs to be done to increase public awareness through methods like social media (51%) and TV campaigns (48%).
- Encourage shared decision making: Although the Panel found that many health professionals do enable shared decision making, this was far from universal. NHS Scotland needs to take action to ensure every health professional in NHS Scotland is committed to shared decision making. Alongside this, there is a need to improve public awareness that shared decision making is normal practice, for example by doing more to promote the “It’s OK to Ask” message.
- Use of BRAN questions: Since 80% of respondents expressed willingness to use the BRAN questions in future interactions with healthcare professionals, NHS Scotland should commit to incorporate reminders about these questions into appointment letters and waiting rooms. A focus on accessible formats would help to ensure access for all.
- Focus on resource management: NHS Scotland should prioritise initiatives aimed at resource optimisation and waste reduction, capitalising on the public’s support for this and desire to be involved. Reducing wasted prescriptions was highlighted by Panel members.
- Improve communication: Many respondents emphasised the need for better communication and listening from healthcare professionals. NHS Scotland must commit to improving communication skills, asking patients for their preferences on how to receive information, and providing patients with clear documentation of decisions and next steps following health care appointments.
NHS Reform
The second section of the survey began by asking respondents for their opinions on NHS Reform:
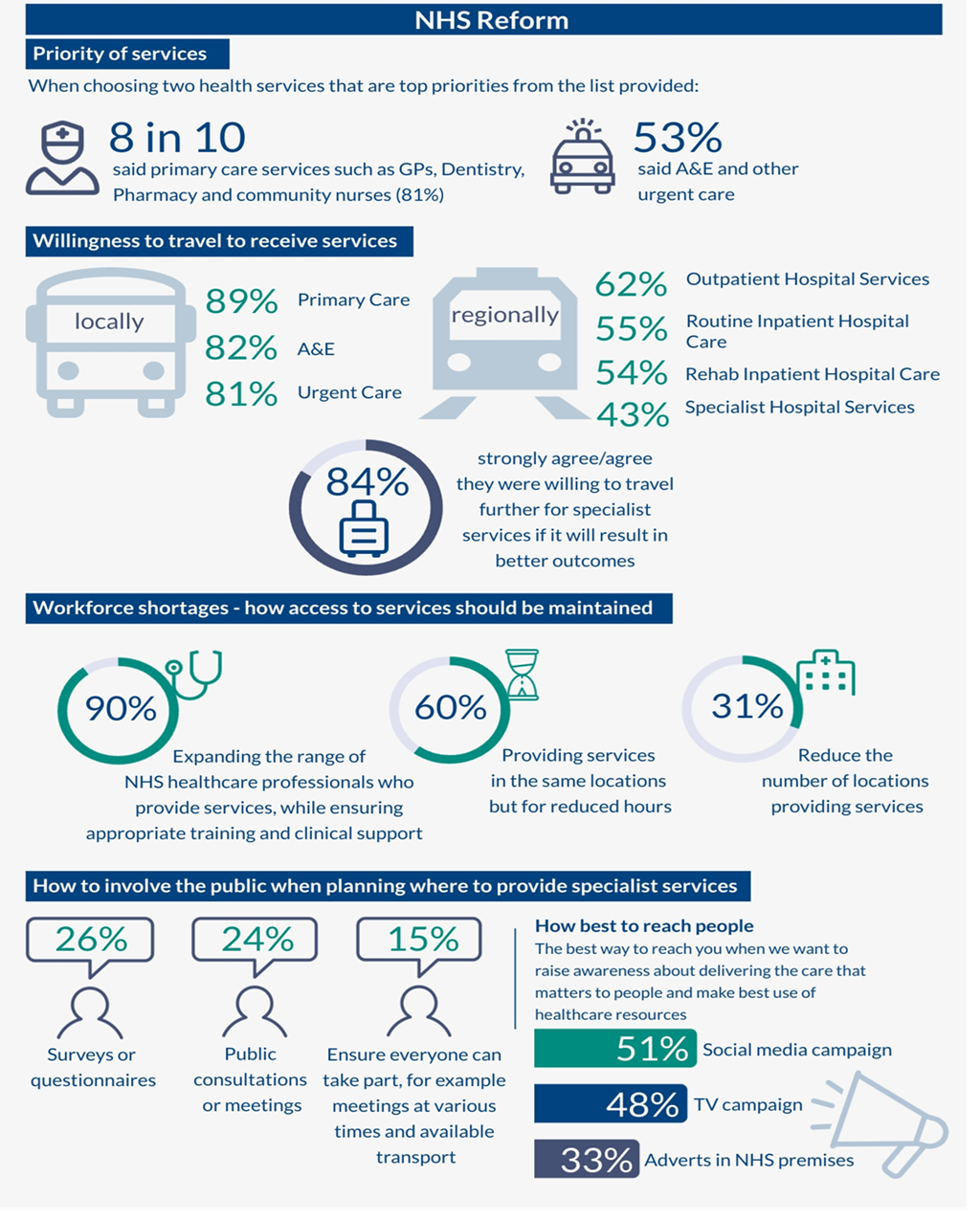
Panel members were asked to choose 2 health services that are top priorities for them from a list provided. Over 8 in 10 respondents said that primary care services such as GPs, dentistry, pharmacy and nurses working in the community was their top or second priority (81%). This was followed by A&E and other urgent care (53%).
It was explained to Panel members that sometimes it is safer to provide services in a specialist unit to ensure a patient receives the highest quality care with the best outcomes. This could be, for example, cancer services, surgery, or dermatology. 84% of respondents strongly agreed or agreed they were willing to travel further for specialist services if it will result in better outcomes for them.
Sometimes it is safer to provide specialised services (such as cancer services, surgery or dermatology) regionally or nationally instead of locally, to ensure patients receive the highest quality care with the best outcomes. When planning for this, NHS Scotland will need to involve the public and listen to their views. An open question was included in the survey which asked Panel members how NHS Scotland should best involve the public in this. Over 1 in 4 respondents (26%) said that surveys or questionnaires should be used to involve the public, 24% suggested more public consultations or meetings and 15% suggested making sure everyone has the opportunity to participate by ensuring that meetings are arranged for various times and transport is available.
Panel members were asked how long they are prepared to travel to receive a range of services. Citizens’ Panel members were most likely to say they would be prepared to travel locally (45 minutes from home on public transport or in what they consider their local area) for primary care services (89%), A&E (82%) and to receive urgent care such as minor injuries or similar (81%). Respondents were most likely to be willing to travel regionally (within 1.5 hours from home) for rehabilitation inpatient hospital care (54%), routine impatient hospital care where a stay in hospital is needed for immediate care (55%) and to access outpatient hospital services (62%). With regards to specialised outpatient and inpatient hospital services, respondents were most likely to say they would be willing to travel regionally (43%), while 33% said they would be willing to travel nationally anywhere in Scotland and 24% said they would only be willing to travel locally to access this type of service.
Finally, respondents were asked about how they think access to services should be maintained when the NHS faces workforce shortages. Respondents were provided with a list of options and asked for their top two preferences. For 9 in 10 respondents (90%) expanding the range of NHS health and care professionals who provide services, while ensuring they have appropriate training and clinical support, was a top or second top priority. This was followed by providing services in the same locations but for reduced hours (60%) and reducing the number of locations at which services are provided.
Recommendations
Based on these findings, we make the following recommendations to the Scottish Government and NHS Scotland:
- Ensure local access to primary care services and urgent care: A reformed NHS Scotland should ensure that the public has access to primary care services such as GPs, dentistry, pharmacy and community nursing at a local level. In addition, urgent care including Accident & Emergency services should be available locally.
- Understand travel willingness: The majority of the public is willing to travel regionally for most hospital services and nationally for some specialised services, where this will result in better outcomes for them. NHS Scotland needs to engage with the public to explore in detail how different models of regional and national services could best deliver care.
- Public involvement in NHS Reform: Respondents were enthusiastic about public involvement in NHS service planning. NHS Scotland should commit to putting public engagement at the heart of reform. This should include a variety of options to maximise opportunities for public involvement, including a national survey, public meetings across Scotland and reaching people through social media and traditional media campaigns.
- Expand the range of health professionals: NHS Reform should continue to build on existing progress to expand the range of health professionals’ roles in multidisciplinary teams. This was supported by 90% of respondents to help alleviate workforce shortages while maximising access to services.
- Address rural healthcare needs: Some respondents highlighted concerns about the impact of centralising services on rural communities. NHS Reform must consider the needs of remote, rural and island populations, including the use of relevant impact assessments.
These recommendations aim to enhance the effectiveness and accessibility of NHS Scotland's services while addressing the concerns raised by the public in the survey.
Impact
Policymakers continue to note the significant impact of this Citizens’ Panel findings.
Insights from the panel report - including the importance of the NHS making better use of resources, reducing waste and delivering care that matters - have informed the Scottish Government Long term conditions framework: consultation analysis (published October 2025) and helped shape the Realistic Medicine workforce survey and Realistic Medicine Casebook (published May 2025). The survey report asked health and care professionals how they will further support shared decision making and encourage people they care for to become more involved in decisions about their care.
At the May 2025 Realistic Medicine Network meeting, members welcomed that the survey results supported the key Realistic Medicine principles and reported that the findings have helped to:
- Strengthen internal presentations and messaging within Health Boards
- Inform ongoing work by Health Boards to standardise patient letters
- Inform planning for coordinated social media campaigns and possible video resources
- Shape an outpatient communication review for one Health Board to inform improvements in patient communication.
The findings have also been used to inform and strengthen the Realistic Medicine component of the Population Health Framework and the Service Renewal Framework, both published in June 2025. These strategic frameworks are designed in line with the Value Based Health and Care principles to deliver outcomes that matter most to the people of Scotland.
The findings from this survey have been presented widely at events and conferences across Scotland and are now embedded in core messaging, featuring prominently in presentations to Health Boards, specialist societies, Medical Colleges, and Scottish Government partners. This reach has extended internationally, with presentations to Integrated Care Boards in NHS England and Ireland. Messaging is reinforced through senior leaders (including the Chief Medical Officer and the Deputy Chief Medical Officer) and press engagement.
Policymakers continue to work with all Health Boards, the Realistic Medicine Network, and other key stakeholders to track progress and drive implementation of recommendations. The survey findings remain central to shaping the policy agenda, strengthening communication, and driving meaningful change across Scotland.