Sixth Panel Report
The sixth Citizens' Panel survey was carried out in January 2020.
We asked questions about antibiotic resistance, access to and use of antibiotics, self-limiting infections and the impact of public health campaigns targeted at managing common infections.
In total, 599 Panel members responded to the survey which represents a 52% response rate. The results will support the work of the Scottish Antimicrobial Prescribing Group (SAPG) which is committed to using the feedback to help engage with, and inform, the public about responsible antibiotic use.
Conclusions and recommendations
The public appear to have relatively good knowledge and behaviours around antibiotic resistance, access and use of antibiotics, self-limiting infections and public health campaigns.
Some suggestions about areas that need more public information and awareness include:
- information about causes of resistance
- more information about which infections are self-limiting and which need treatment, and
- reinforcing advice on self-care for self-limiting infections.
Campaigns designed to increase public understanding of antimicrobial resistance should emphasise that it is bacteria that become resistant to antibiotics not individuals.
Further emphasis should also be made that antibiotics are effective only for the treatment of bacterial infections not viral infections.
The results will support the work of the SAPG to help engage with and inform patients and the public about responsible antibiotic use.
Key findings
Antibiotic resistance
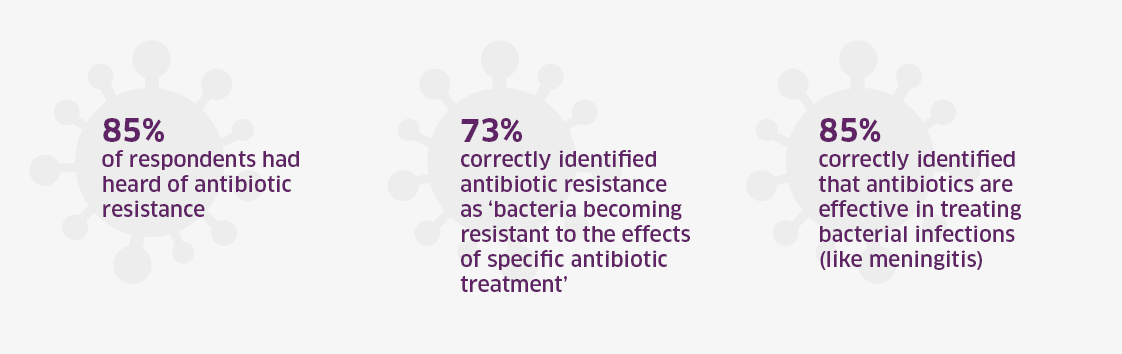
85% of respondents had heard of antibiotic resistance.
73% correctly identified antibiotic resistance as 'bacteria becoming resistant to the effects of specific antibiotic
treatment'.
85% correctly identified that antibiotics are effective in treating bacterial infections (like meningitis).
Panel members were more aware of some factors that contribute to antibiotic resistance than others:
- Prescribing antibiotics when not required (92%)
- Patients not completing a prescribed course of antibiotics (61%)
- Incorrect antibiotic or dosage (50%)
- Use of antibiotics to promote growth in animals (38%)
- Contamination of water from human or animal waste (18%)
Personal experience of using antibiotics
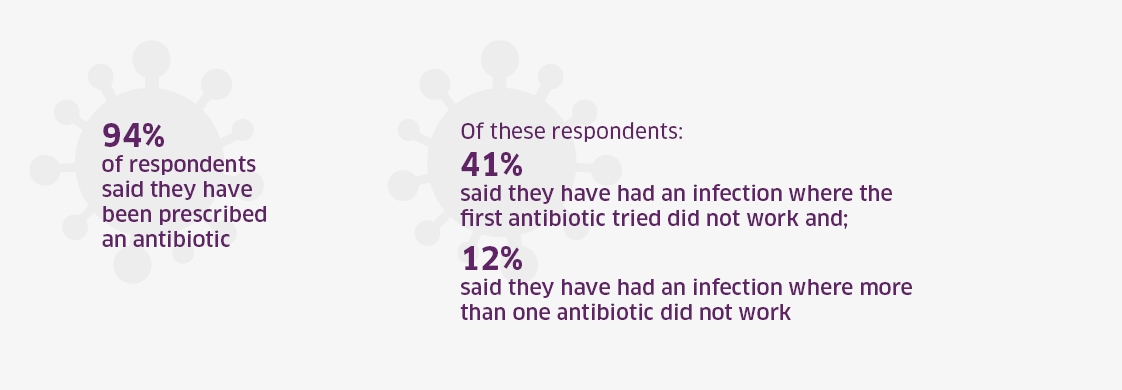
94% of respondents said they have been prescribed an antibiotic.
Of these respondents, 41% said they have had an infection where the first antibiotic tried did not work. 12%
said they have had an infection where more than one antibiotic did not work.
Those who said they were prescribed an antibiotic which did not work in the first instance were asked why this was the case. The top 3 reasons provided were:
- Not the right type of antibiotic for infection (41%)
- Was not strong enough (21%)
- Don't know (19%)
Self-limiting infections
SAPG sought Panel Members' views on self-limiting infections – which will clear up on their own – and how these should be treated.
The majority of respondents correctly agreed with the following statements:
- Symptoms of self-limiting infections can be helped by resting, drinking fluids and taking paracetamol (94%)
- The common cold is a self-limiting infection (81%)
- Self-limiting infections will get better without antibiotics (76%)
- Using antibiotics for self-limiting infections contributes to antibiotic resistance (71%)
The majority correctly disagreed with the following statements:
- A sore throat is not self-limiting and needs antibiotic treatment (67%)
- Pneumonia is a self-limiting infection (64%)
In relation to ear infections in young children, 42% of respondents said these are rarely self-limiting so antibiotics should be used, 10% disagreed, 16% neither agreed nor disagreed and 33% were uncertain. Ear infections are usually self-limiting in young children and the correct response was to disagree with antibiotic use.
The impact of public health campaigns
"Keep antibiotics working"
- 57% of respondents had seen the campaign.
- The GP or health centre was the most common place people had seen this information (43%).
- 90% of respondents obtain information from qualified healthcare professionals such as a doctor, nurse or pharmacist.
- In terms of obtaining information about antibiotics:
- 43% from antibiotic packaging leaflets.
- 35% from online NHS sources.
- 30% from public awareness campaigns.
- In terms of how respondents assess the reliability of the information they receive:
- 28% stated that they only consult professionals e.g. pharmacist, doctor, nurse.
- 28% stated they trust NHS sources.
- 20% stated that they trust their GP's knowledge.
Spotting the signs of dehydration
- 37% of respondents were aware of the campaign, which seeks to highlight the importance of staying hydrated to minimise the risk of developing a urinary infection and maintaining good health.
- The most popular place to have observed this message was at GP or health centres (24%).
- In terms of fluid consumption, responses ranged from 1 litre to 10 litres with a mean score of 2.36 litres. This indicates that people are aware of how much fluids they should be consuming. The recommended amount is to drink 6 to 8 mugs of fluid, the equivalent to roughly 1.5 to 2 litres, although this varies according to heat, activity and wellness.
- Almost all respondents knew if they were well hydrated their urine would be light in colour (97%) and that if they were dehydrated their urine would be dark in colour (96%).
"Pharmacy first" service
- 54% of respondents were aware of the service, which provides treatment of common infections via pharmacies.
- More than 1 in 4 respondents (27%) had used the service.
- 87% were comfortable seeking advice from a pharmacist.
- 89% were comfortable taking the advice they had been given from the pharmacist.
- 72% were comfortable taking antibiotic treatment prescribed by a pharmacist.